Blog
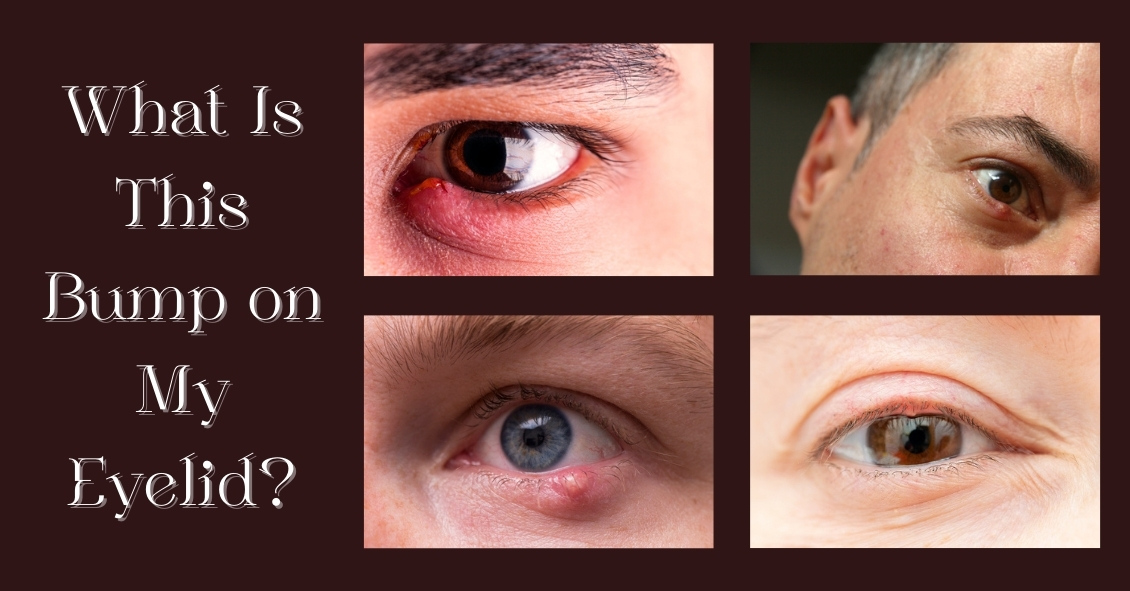
So you’re going about your day and notice a slight twinge when you blink. It starts off as a mild awareness, then proceeds to a painful feeling with every blink. You look in the mirror to see what could be causing it, and there you see a small...

Itching, burning, watering, red, irritated, tired eyes... what is a person to do? These symptoms are classic signs of Dry Eye Syndrome (DES), which affects millions of adults and children.
What causes this? Dry eye syndrome can be brought on...

